Evicore Appeal Form
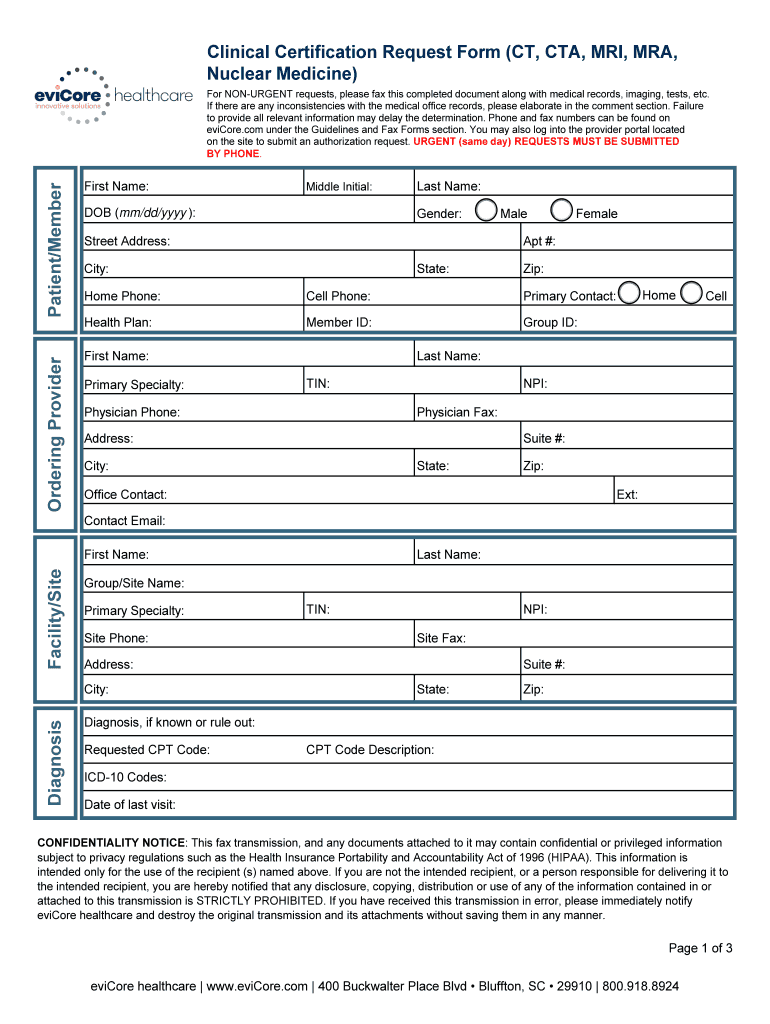
Evicore Appeal Form - Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. • providers may provide additional information and request reconsideration from evicore. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. For evicore by evernorth® appeals, review your appeal denial letter for instructions. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. The request submission form should be used for denied cases. Please ensure you are navigating to our most. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed.
For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The request submission form should be used for denied cases. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. • providers may provide additional information and request reconsideration from evicore. Please ensure you are navigating to our most. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. For evicore by evernorth® appeals, review your appeal denial letter for instructions.
• providers may provide additional information and request reconsideration from evicore. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The request submission form should be used for denied cases. Please ensure you are navigating to our most. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. For evicore by evernorth® appeals, review your appeal denial letter for instructions.
Fill Free fillable eviCore PDF forms
Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Please ensure you are navigating to our most. The request submission form should be used for denied cases. Appeal requests for priority partners members must be.
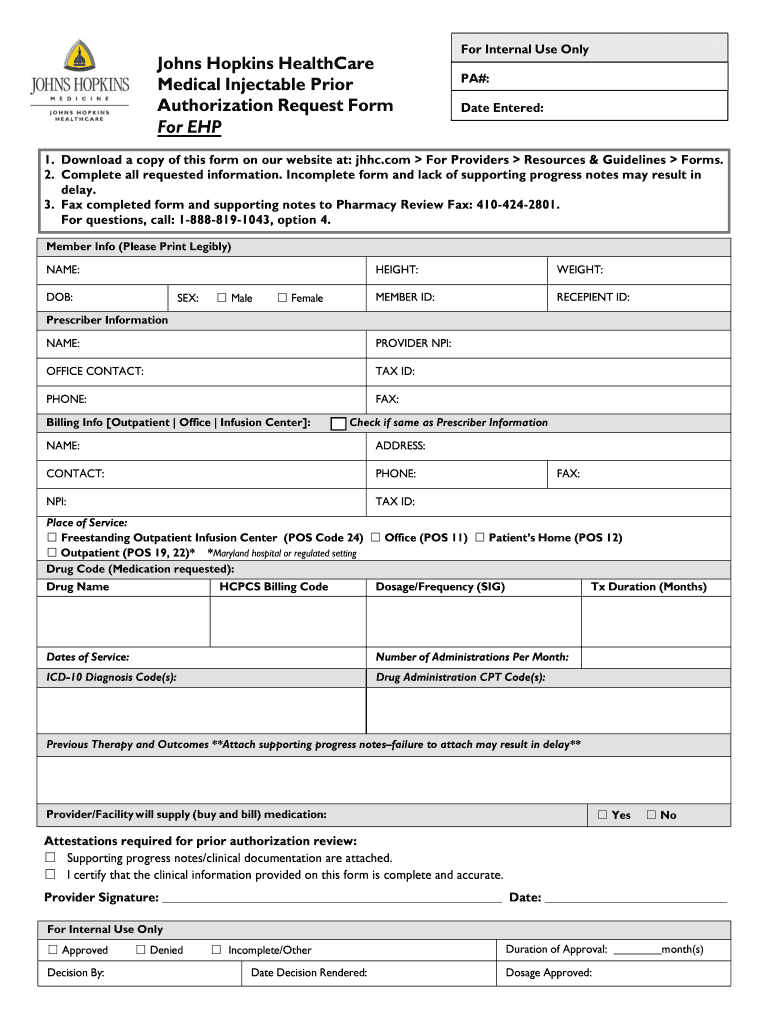
Johns Hopkins Authorization Request Form Fill Online, Printable
The request submission form should be used for denied cases. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. • providers may provide additional information and request reconsideration from evicore. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. Please ensure you are.
Understanding EviCore's Approach to PatientCentered Care eviCore
• providers may provide additional information and request reconsideration from evicore. For evicore by evernorth® appeals, review your appeal denial letter for instructions. The request submission form should be used for denied cases. Please ensure you are navigating to our most. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed.
Fill Free fillable eviCore PDF forms
Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. The request submission form should.
Fillable Online Evicore cigna prior authorization form Fax Email Print
Please ensure you are navigating to our most. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. • providers may provide additional information and request reconsideration from evicore. For evicore by evernorth® appeals, review your appeal denial letter for instructions. Appeal requests for priority partners members must.
Cigna reconsideration form Fill out & sign online DocHub
The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. For evicore by evernorth® appeals, review your appeal denial letter for instructions. For example, use the prior authorization general request form below if you would like.
Fill Free fillable eviCore PDF forms
For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Appeal requests.
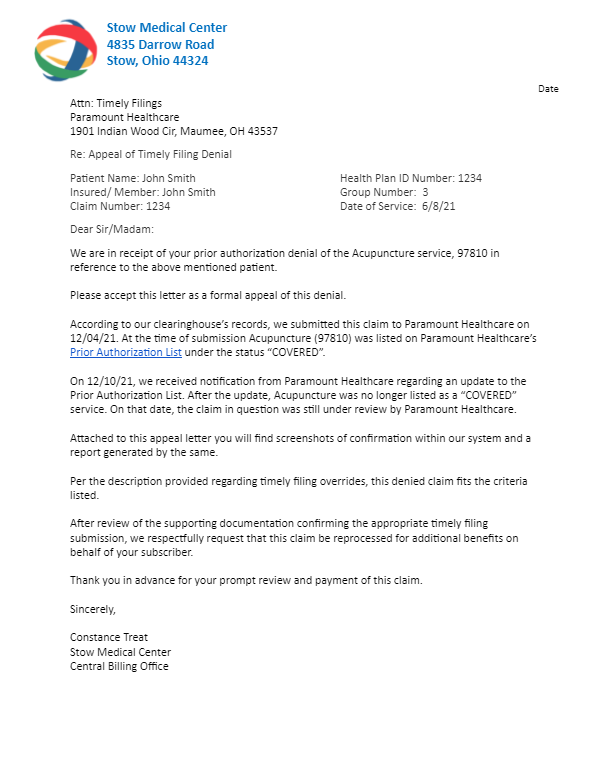
46+ Unitedhealthcare Appeal Letter Sample TanayaMeryl
Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. For evicore by evernorth® appeals, review your appeal denial letter for instructions. Please ensure you are navigating to our most. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. Formal appeal the letter you receive will also outline.
EviCore Healthcare Lymphedema Program PT/OT Therapy Intake Form 2020
For evicore by evernorth® appeals, review your appeal denial letter for instructions. Please ensure you are navigating to our most. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. • providers may provide additional information and request reconsideration.
Evicore Certification Request Form Fill Online, Printable, Fillable
The request submission form should be used for denied cases. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be.
• Providers May Provide Additional Information And Request Reconsideration From Evicore.
Please ensure you are navigating to our most. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. The request submission form should be used for denied cases.
Evicore.com Recently Upgraded And Some Of Your Bookmarked Worksheets Might Have Changed.
For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan.

.png)