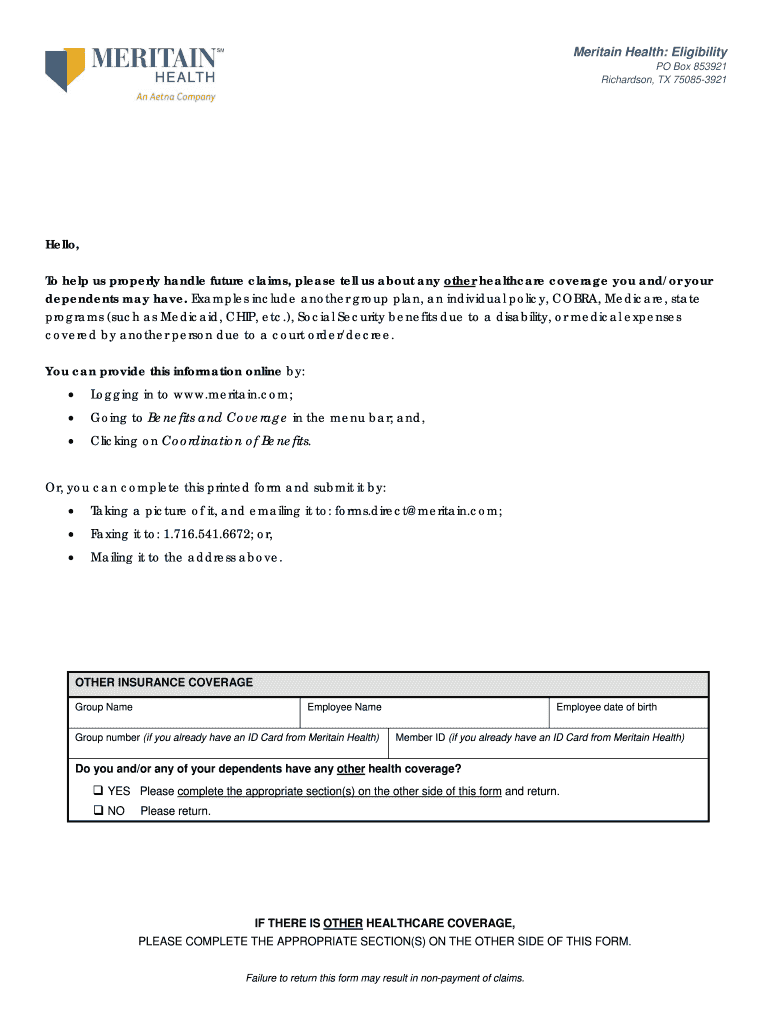
Meritain Prior Authorization Form
Meritain Prior Authorization Form - Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Always place the predetermination request form on top of other supporting documentation. **please select one of the options at the left to proceed with your request. Contact your meritain health® representative. Welcome to the meritain health benefits program. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. This file provides crucial instructions for completing the coverage determination request form. Surgery should not be scheduled prior to determination of coverage. Always verify eligibility and benefits first. It includes member and provider.
Always verify eligibility and benefits first. It includes member and provider. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Please include any additional comments if needed with. Surgery should not be scheduled prior to determination of coverage. Contact your meritain health® representative. Always place the predetermination request form on top of other supporting documentation. Welcome to the meritain health benefits program. This file provides crucial instructions for completing the coverage determination request form. **please select one of the options at the left to proceed with your request.
Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. This file provides crucial instructions for completing the coverage determination request form. Always place the predetermination request form on top of other supporting documentation. It includes member and provider. Always verify eligibility and benefits first. Surgery should not be scheduled prior to determination of coverage. **please select one of the options at the left to proceed with your request. Please include any additional comments if needed with. Contact your meritain health® representative.
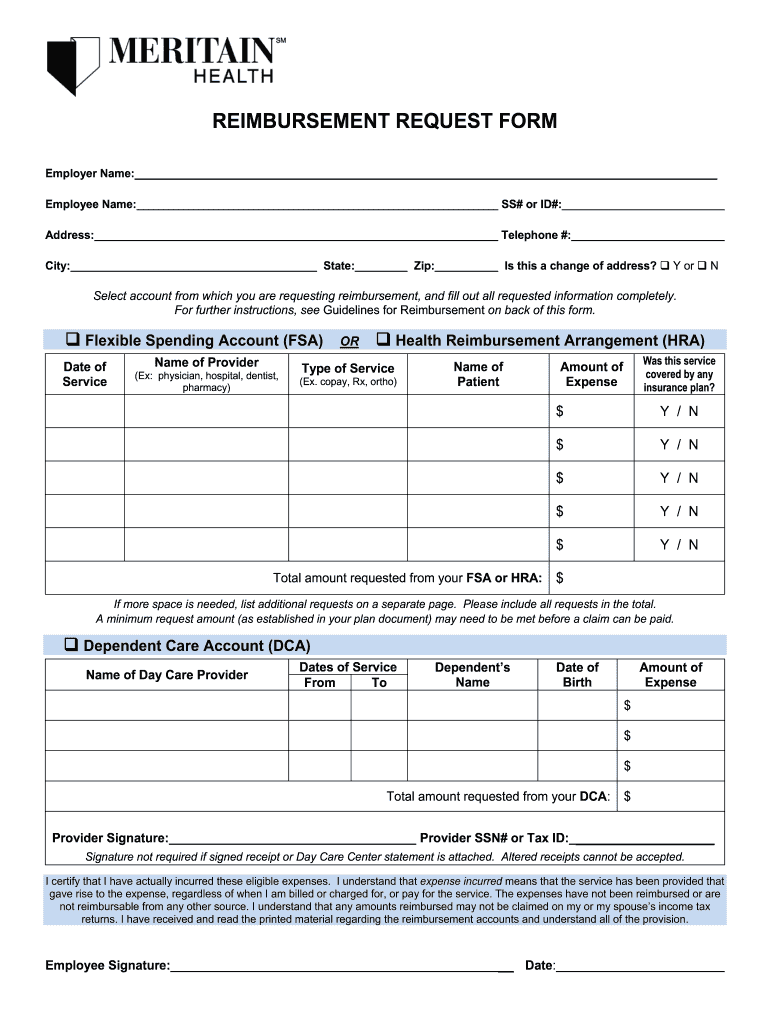
Meritain Med Necessity 20192024 Form Fill Out and Sign Printable PDF
Welcome to the meritain health benefits program. **please select one of the options at the left to proceed with your request. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Always place the predetermination request form on top of other supporting documentation. Meritain health’s® medical management program is designed to.
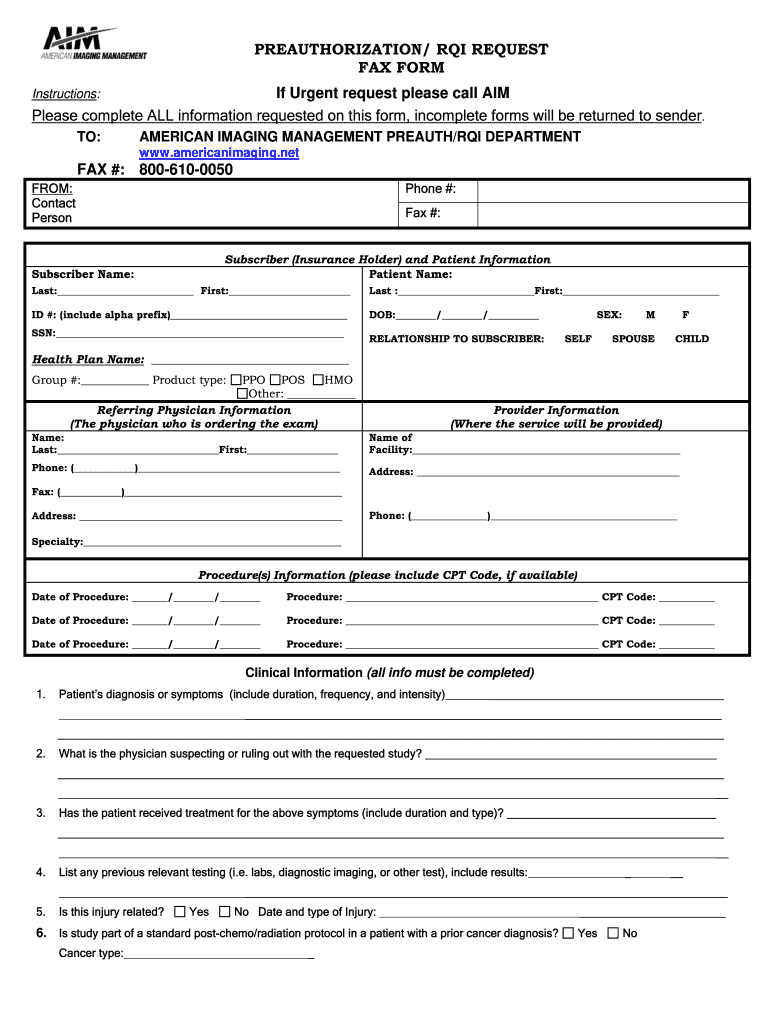
Aims Form Printable Printable Forms Free Online
Surgery should not be scheduled prior to determination of coverage. **please select one of the options at the left to proceed with your request. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Please include any additional comments if needed with. Percertification and preauthorization (also known as “prior.
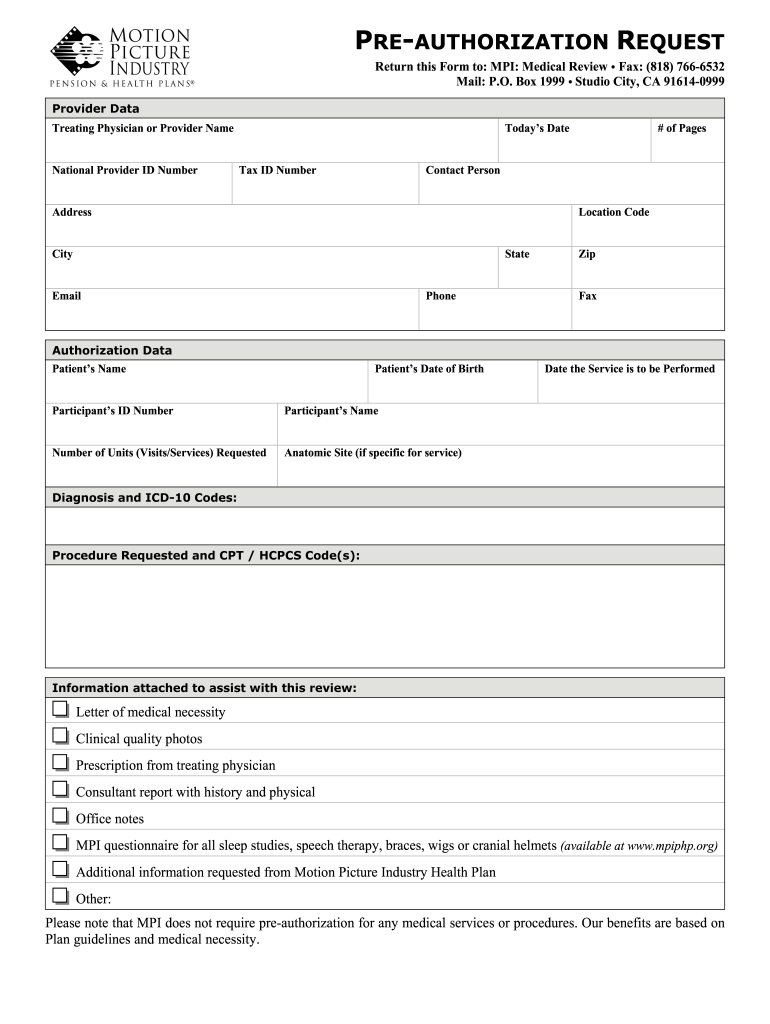
Mpi Authorization Form Fill Online, Printable, Fillable, Blank
Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Always place the predetermination request form on top of other supporting documentation. This file provides crucial instructions for completing the coverage determination request form. Welcome to the meritain health benefits program. Surgery should not be scheduled prior to determination of coverage.
Perfect Info About Authorization Letter Sample Example Resume For
**please select one of the options at the left to proceed with your request. Surgery should not be scheduled prior to determination of coverage. Please include any additional comments if needed with. Welcome to the meritain health benefits program. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you.
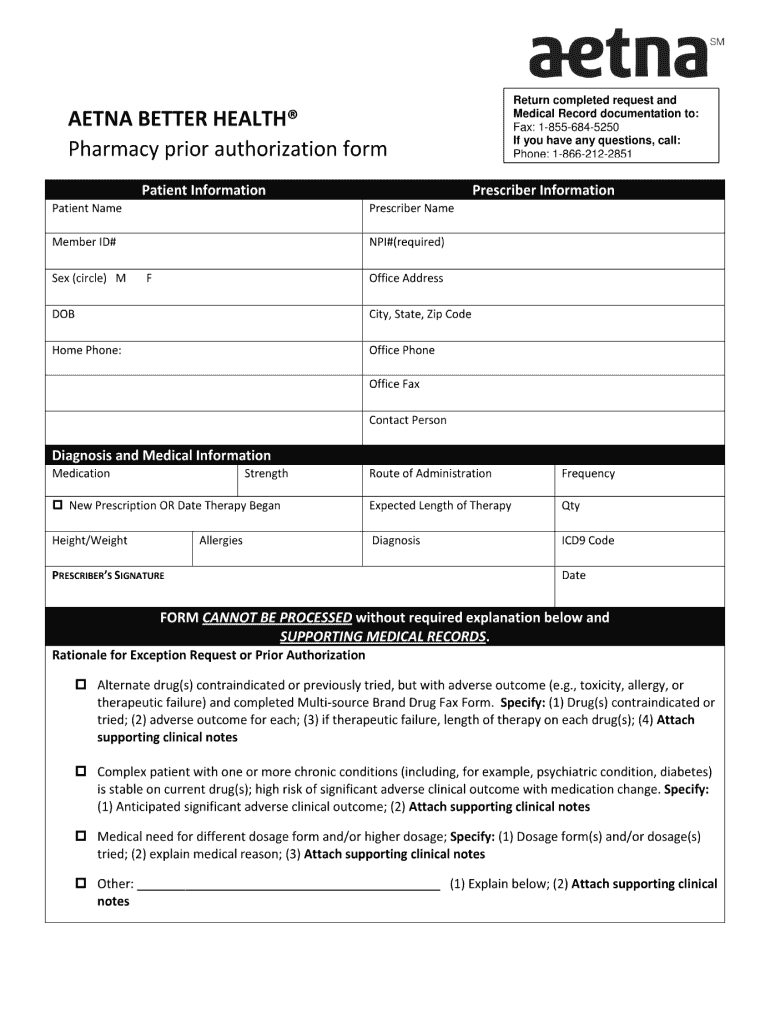
Aetna Precert Tool 20062024 Form Fill Out and Sign Printable PDF
Contact your meritain health® representative. Always verify eligibility and benefits first. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Please include any additional comments if needed with.
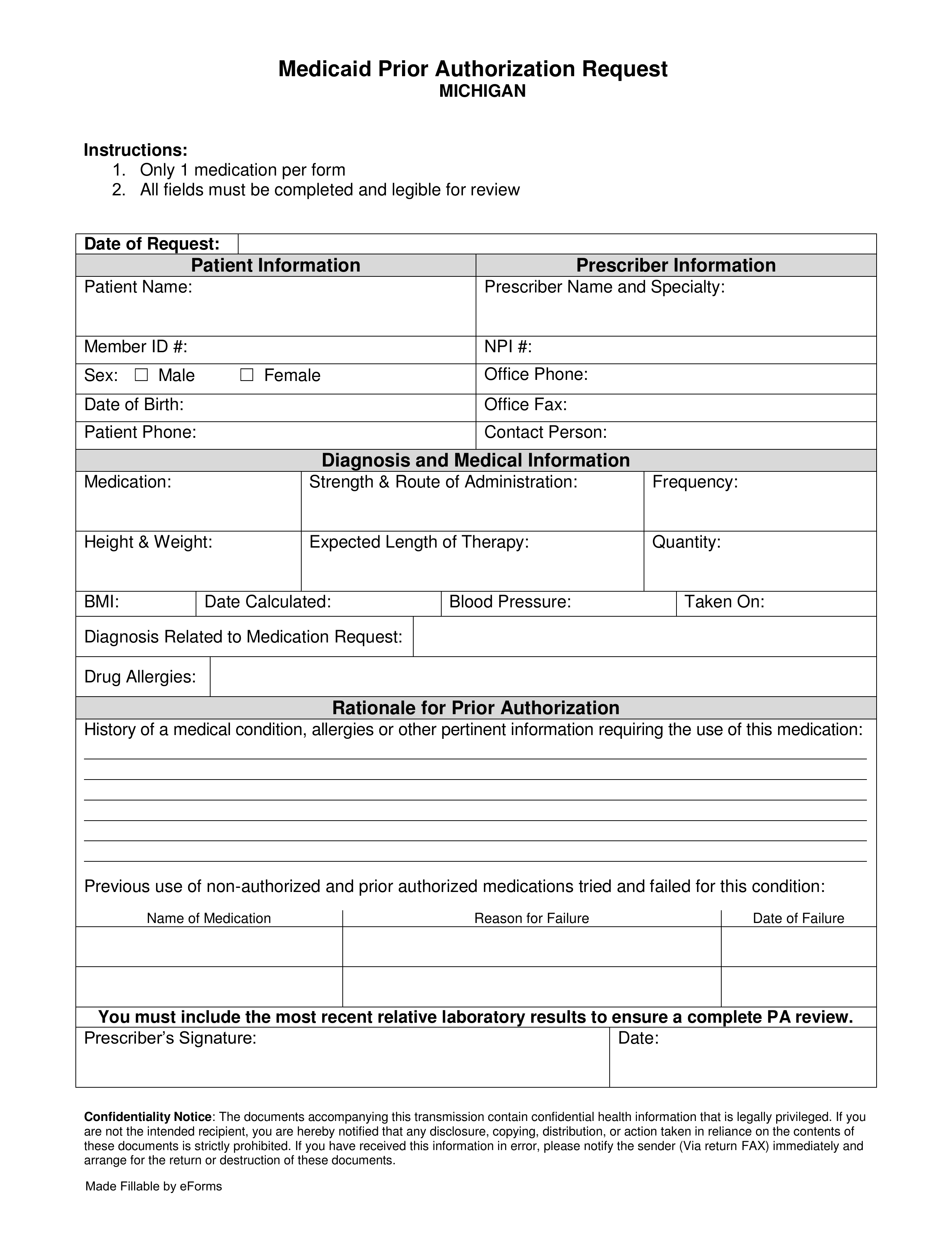
Free Michigan Medicaid Prior (Rx) Authorization Form PDF eForms
Always place the predetermination request form on top of other supporting documentation. Surgery should not be scheduled prior to determination of coverage. It includes member and provider. Please include any additional comments if needed with. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you.
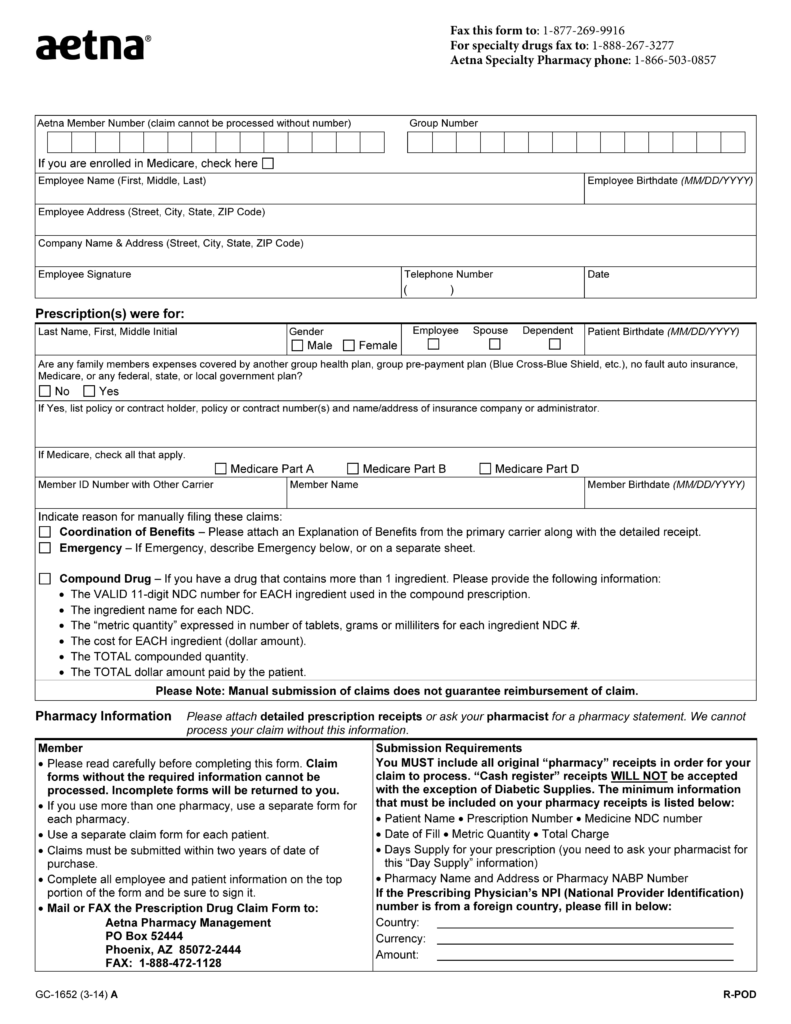
Free Aetna Prior (Rx) Authorization Form PDF eForms
**please select one of the options at the left to proceed with your request. Please include any additional comments if needed with. This file provides crucial instructions for completing the coverage determination request form. Contact your meritain health® representative. Always place the predetermination request form on top of other supporting documentation.
Meritain health prior authorization Fill out & sign online DocHub
Always place the predetermination request form on top of other supporting documentation. Welcome to the meritain health benefits program. Please include any additional comments if needed with. Surgery should not be scheduled prior to determination of coverage. Always verify eligibility and benefits first.
Free Aetna Prior (Rx) Authorization Form PDF eForms
Always verify eligibility and benefits first. It includes member and provider. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Surgery should not be scheduled prior to determination of coverage. **please select one of the options at the left to proceed with your request.
Fillable Online Prior Authorization Criteria Form Fax Email Print
**please select one of the options at the left to proceed with your request. Surgery should not be scheduled prior to determination of coverage. Welcome to the meritain health benefits program. Please include any additional comments if needed with. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you.
This File Provides Crucial Instructions For Completing The Coverage Determination Request Form.
It includes member and provider. **please select one of the options at the left to proceed with your request. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while.
Contact Your Meritain Health® Representative.
Welcome to the meritain health benefits program. Always verify eligibility and benefits first. Please include any additional comments if needed with. Always place the predetermination request form on top of other supporting documentation.