Molina Prior Authorization Request Form
Molina Prior Authorization Request Form - • claims submission and status • authorization submission and status • member. Prior authorization is not a guarantee of payment for services. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health. Pick your state and your preferred language to continue. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Texas standardized prior authorization request form for healthcare. Find out if you can become a member of the molina family.
Find out if you can become a member of the molina family. Pick your state and your preferred language to continue. • claims submission and status • authorization submission and status • member. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health. Prior authorization is not a guarantee of payment for services. Texas standardized prior authorization request form for healthcare. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical.
Prior authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. • claims submission and status • authorization submission and status • member. Texas standardized prior authorization request form for healthcare. Pick your state and your preferred language to continue. Find out if you can become a member of the molina family. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health.
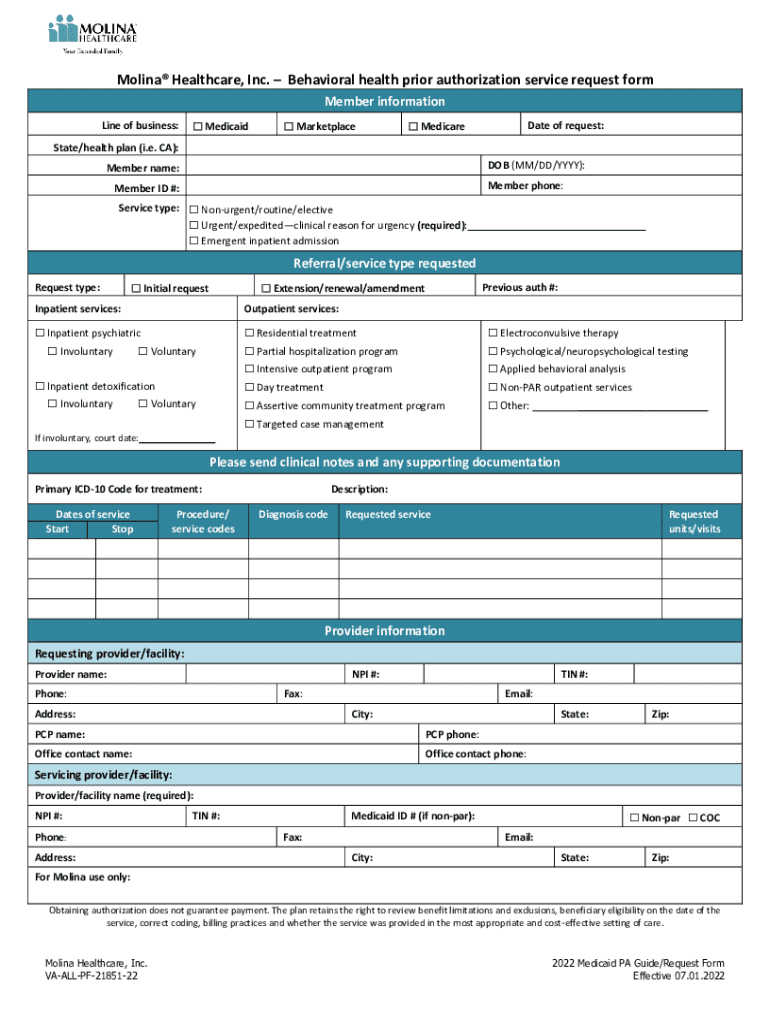
Molina Healthcare Prior Authorization Service Request Form
Texas standardized prior authorization request form for healthcare. Prior authorization is not a guarantee of payment for services. Pick your state and your preferred language to continue. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request.
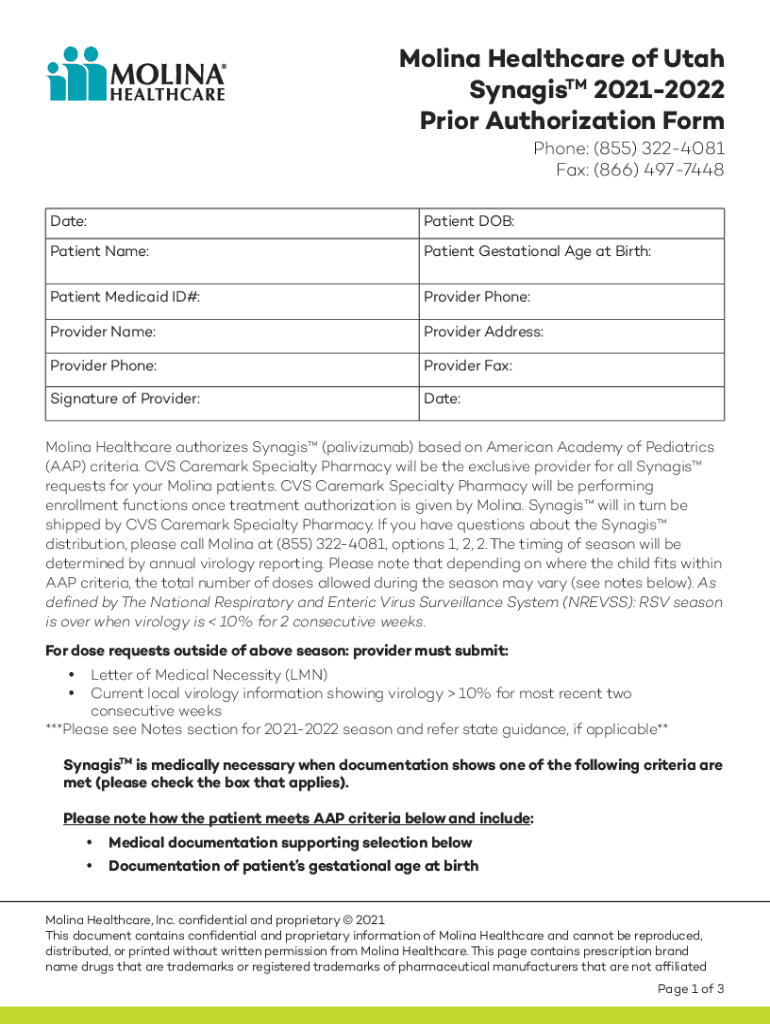
Fillable Online Molina Healthcare of Utah Prior Authorization Request
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health. Prior authorization is not a guarantee of payment for services. Pick your state.
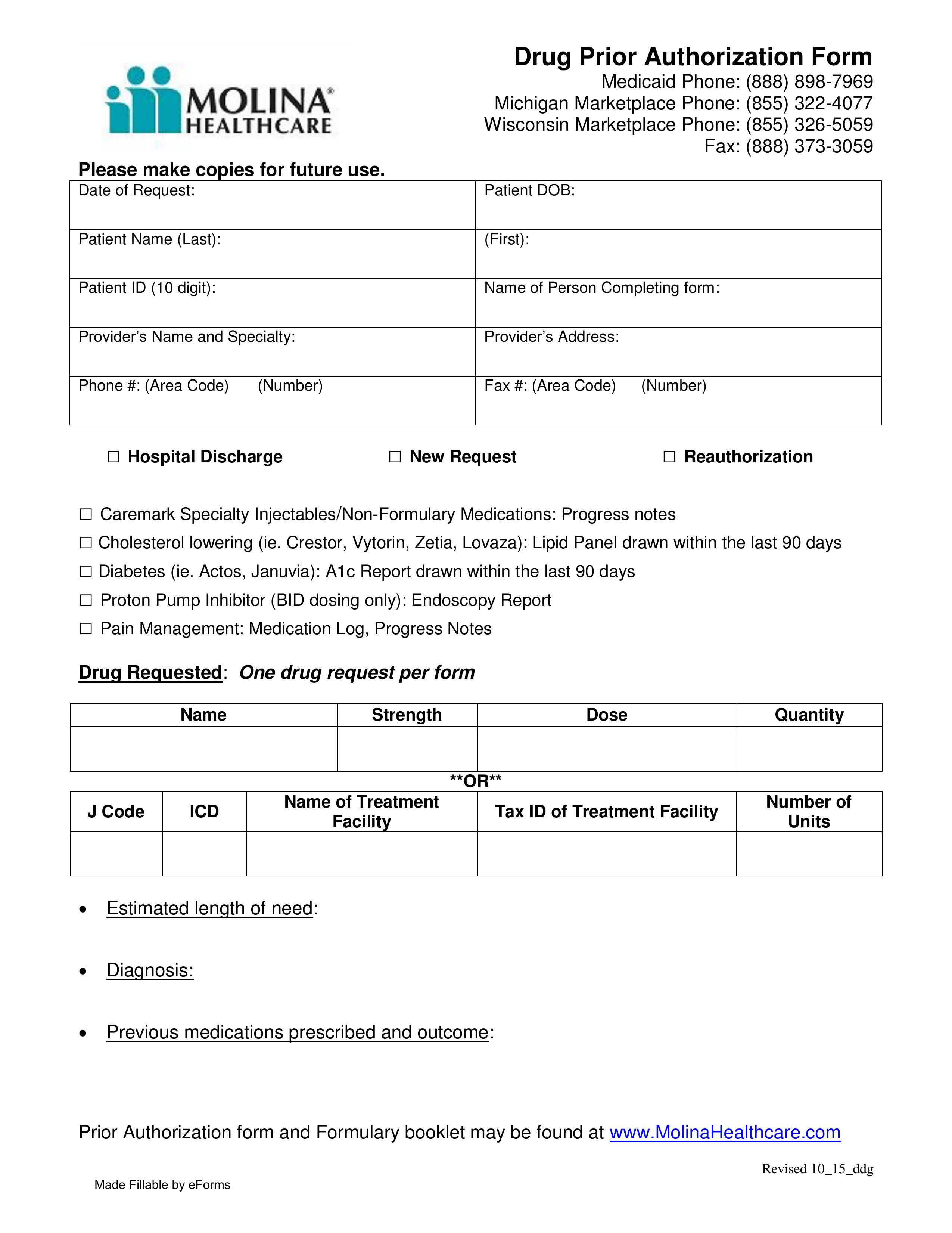
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Prior authorization is not a guarantee of payment for services. Find out if you can become a member of the molina family. Texas standardized prior authorization request form for healthcare. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard.
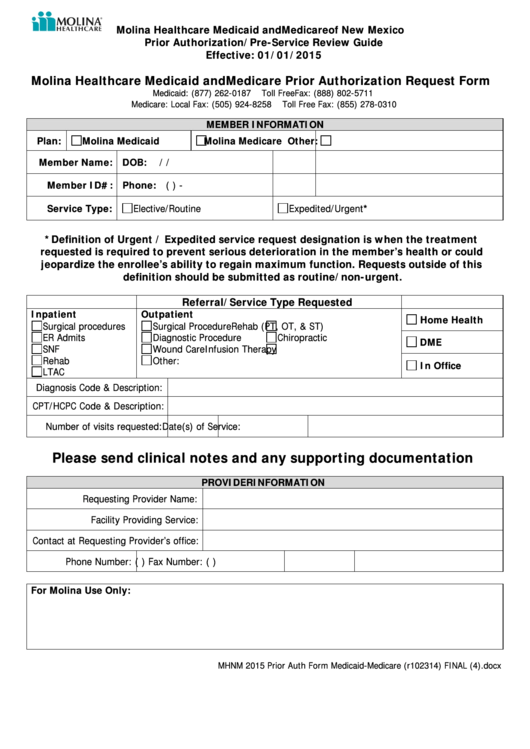
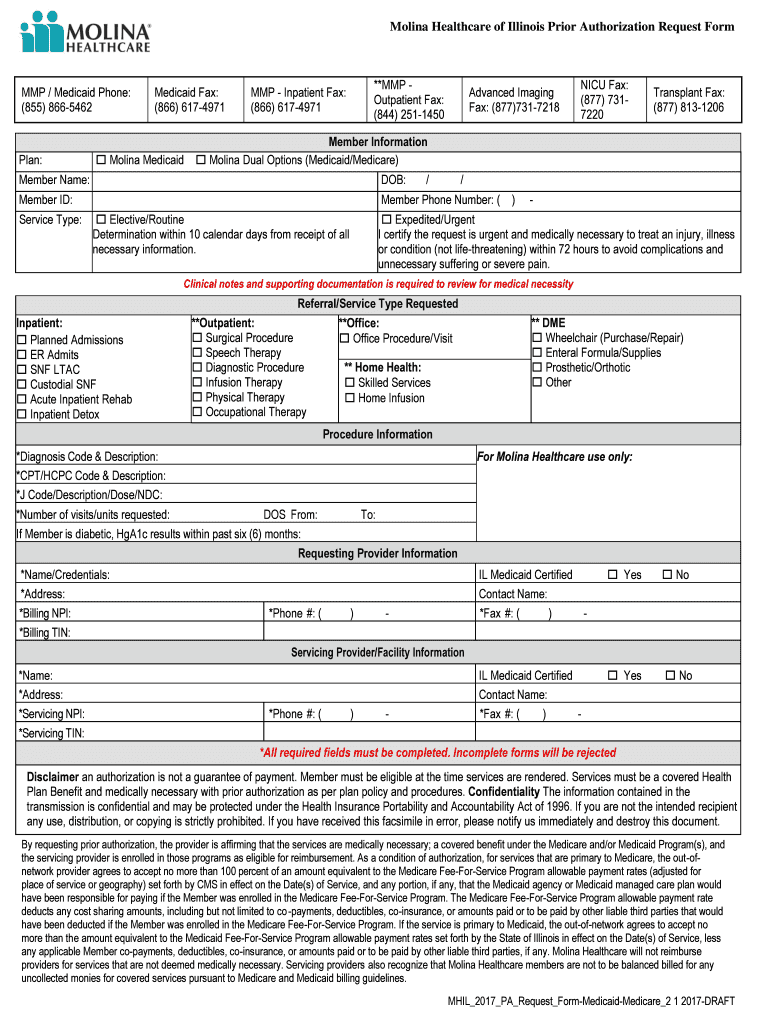
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Find out if you can become a member of the molina family. Texas standardized prior authorization request form for healthcare. • claims submission and status • authorization submission and status • member. Pick your state and your preferred language to continue.
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Prior authorization is not a guarantee of payment for services. Find out if you can become a member of the molina family. • claims submission and status • authorization submission and status • member. Beginning september 1, 2015, health benefit plan issuers must.
Fillable Online Molina Healthcare/Molina Medicare Prior Authorization
Prior authorization is not a guarantee of payment for services. Find out if you can become a member of the molina family. Pick your state and your preferred language to continue. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a.
Fillable Online Molina Healthcare Prior Authorization Service Request
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Prior authorization is not a guarantee of payment for services. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health. Pick your state.
Fillable Online Molina Healthcare, Inc.Behavioral health prior
• claims submission and status • authorization submission and status • member. Find out if you can become a member of the molina family. Texas standardized prior authorization request form for healthcare. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Beginning september 1, 2015, health benefit plan issuers must accept the.
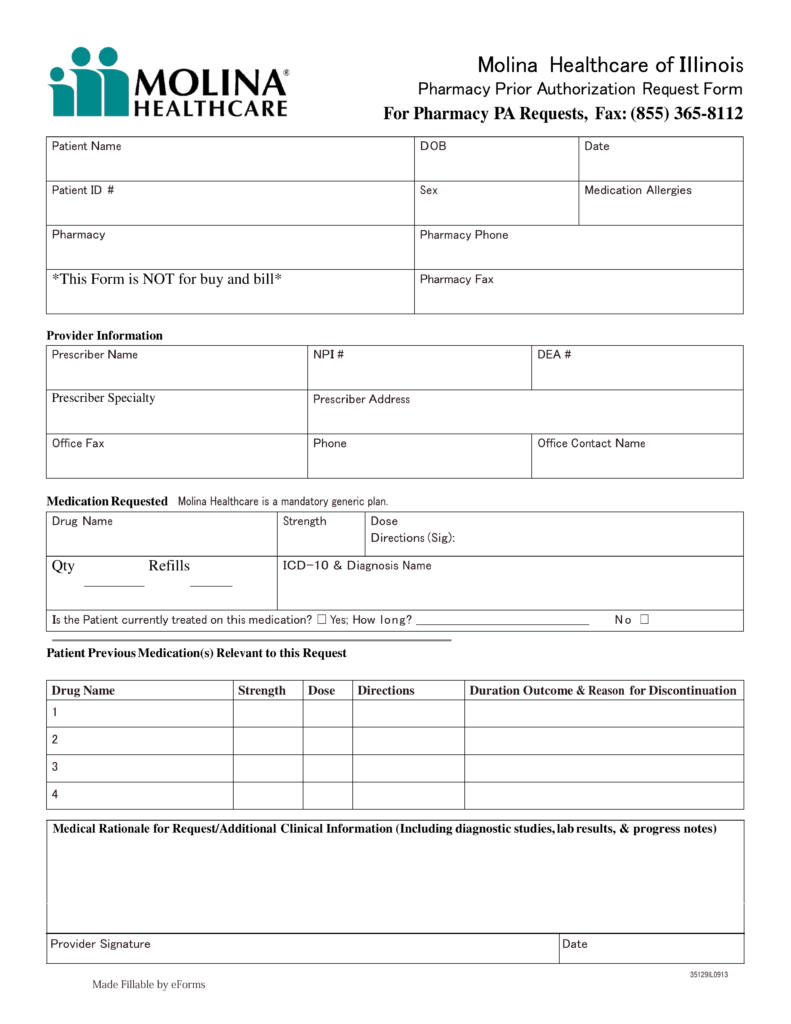
Fillable Online Molina Healthcare of Illinois Prior Authorization
• claims submission and status • authorization submission and status • member. Prior authorization is not a guarantee of payment for services. Pick your state and your preferred language to continue. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a.
Michigan Molina Prior Authorization PDF Form FormsPal
Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health. Texas standardized prior authorization request form for healthcare. • claims submission and status • authorization submission and status • member. Find out if you can become a member of the.
Payment Is Made In Accordance With A Determination Of The Member’s Eligibility, Benefit Limitation/Exclusions, Evidence Of Medical.
• claims submission and status • authorization submission and status • member. Find out if you can become a member of the molina family. Texas standardized prior authorization request form for healthcare. Prior authorization is not a guarantee of payment for services.
Beginning September 1, 2015, Health Benefit Plan Issuers Must Accept The Texas Standard Prior Authorization Request Form For Health Care Services If The Plan Requires Prior Authorization Of A Health.
Pick your state and your preferred language to continue.